- Solutions
- Accounting
- Additional Documentation Requests (ADRs) Management & Support
- Clinical Consulting
- EHR Implementation & Optimization
- Medicaid Eligibility
- Outsourced Contract Controller Services
- Outsourced Revenue Cycle Management
- PointClickCare® Consulting
- QAPI Consulting
- Resident Trust Fund Management & Advisory Services
- Revenue Cycle and Reimbursement Consulting
- Who We Serve
- Resources
- Careers
- About Us
- Contact

 The new Section GG will be in effect on October 1, 2016 for Long Term Care Facilities using the MDS 3.0 for payment. Although the new Resident Assessment Instrument (RAI) manual has not been released, we are able to extrapolate the majority of the information from our LTAC cousins who are already using this new section. The purpose of the new section is to make it possible to measure the function of a resident across the entire post-acute care continuum. In order to do this it was necessary for the questions being asked to be worded in the same way to provide consistency. The new Section GG item set will be added to the 5 Day PPS Assessment as well as the Discharge Assessment for all traditional Medicare A residents. There will also be a new assessment for those traditional Medicare A residents who are discontinued from skilled services, but remain in the long term care facility. This assessment will be called a “Discharge Form Medicare Assessment.”
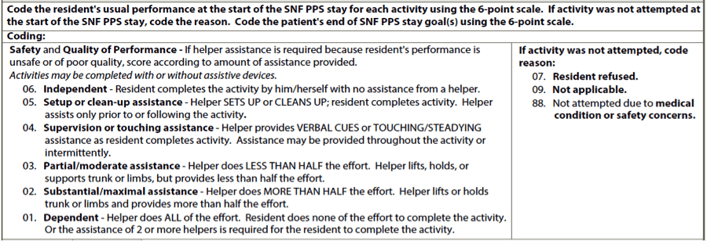
The new Section GG will be in effect on October 1, 2016 for Long Term Care Facilities using the MDS 3.0 for payment. Although the new Resident Assessment Instrument (RAI) manual has not been released, we are able to extrapolate the majority of the information from our LTAC cousins who are already using this new section. The purpose of the new section is to make it possible to measure the function of a resident across the entire post-acute care continuum. In order to do this it was necessary for the questions being asked to be worded in the same way to provide consistency. The new Section GG item set will be added to the 5 Day PPS Assessment as well as the Discharge Assessment for all traditional Medicare A residents. There will also be a new assessment for those traditional Medicare A residents who are discontinued from skilled services, but remain in the long term care facility. This assessment will be called a “Discharge Form Medicare Assessment.”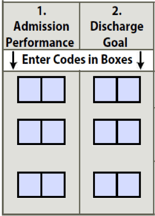 charge planning should begin on day 1 of admission. When coding for Section GG, you will be coding “usual performance”, which is very different that how we currently code for section G. Section GG is asking a very different question. ‘What is the resident most of the time?” This question will require an in depth look at the residents ADL’s as well as interviewing staff on 3 shifts and multiple disciplines in order to answer the questions completely. It is imperative that you fully complete the Discharge Goal column for the purpose of Quality Measures. One of the new Quality Measures will specifically ask whether the resident goals were set on admission. The information will be gathered directly to Section GG of the MDS.
charge planning should begin on day 1 of admission. When coding for Section GG, you will be coding “usual performance”, which is very different that how we currently code for section G. Section GG is asking a very different question. ‘What is the resident most of the time?” This question will require an in depth look at the residents ADL’s as well as interviewing staff on 3 shifts and multiple disciplines in order to answer the questions completely. It is imperative that you fully complete the Discharge Goal column for the purpose of Quality Measures. One of the new Quality Measures will specifically ask whether the resident goals were set on admission. The information will be gathered directly to Section GG of the MDS.