- Solutions
- Accounting
- Additional Documentation Requests (ADRs) Management & Support
- Clinical Consulting
- EHR Implementation & Optimization
- Medicaid Eligibility
- Outsourced Contract Controller Services
- Outsourced Revenue Cycle Management
- PointClickCare® Consulting
- QAPI Consulting
- Resident Trust Fund Management & Advisory Services
- Revenue Cycle and Reimbursement Consulting
- Who We Serve
- Resources
- Careers
- About Us
- Contact

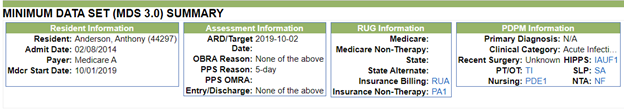
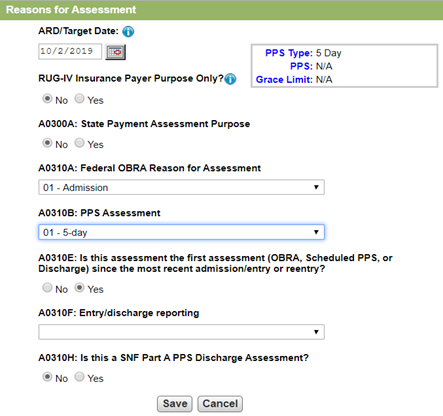
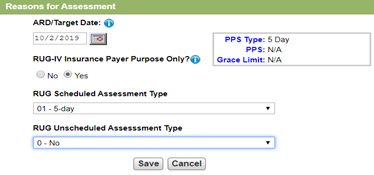
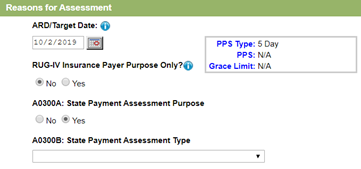
.jpg?width=300&name=IMAGE%7B3%7D%20What%20Your%20LTPAC%20Should%20Do%20About%20Medicare%20Advantage%20Plans%20Under%20PDPM%20(ID%20145122).jpg) In the months leading up to October 1, 2019, providers across the long-term post-acute care (LTPAC) spectrum have been very busy preparing for PDPM for Medicare A residents. We at Richter have as well, as we’ve been training, updating software, adjusting processes and planning our strategy for the biggest change in reimbursement in over 20 years. The good news: It’s finally here! The bad news: There is no real direction on what to do about Medicare Advantage plans.
In the months leading up to October 1, 2019, providers across the long-term post-acute care (LTPAC) spectrum have been very busy preparing for PDPM for Medicare A residents. We at Richter have as well, as we’ve been training, updating software, adjusting processes and planning our strategy for the biggest change in reimbursement in over 20 years. The good news: It’s finally here! The bad news: There is no real direction on what to do about Medicare Advantage plans.